by: Mohamed Yaghi and Husam Yaghi
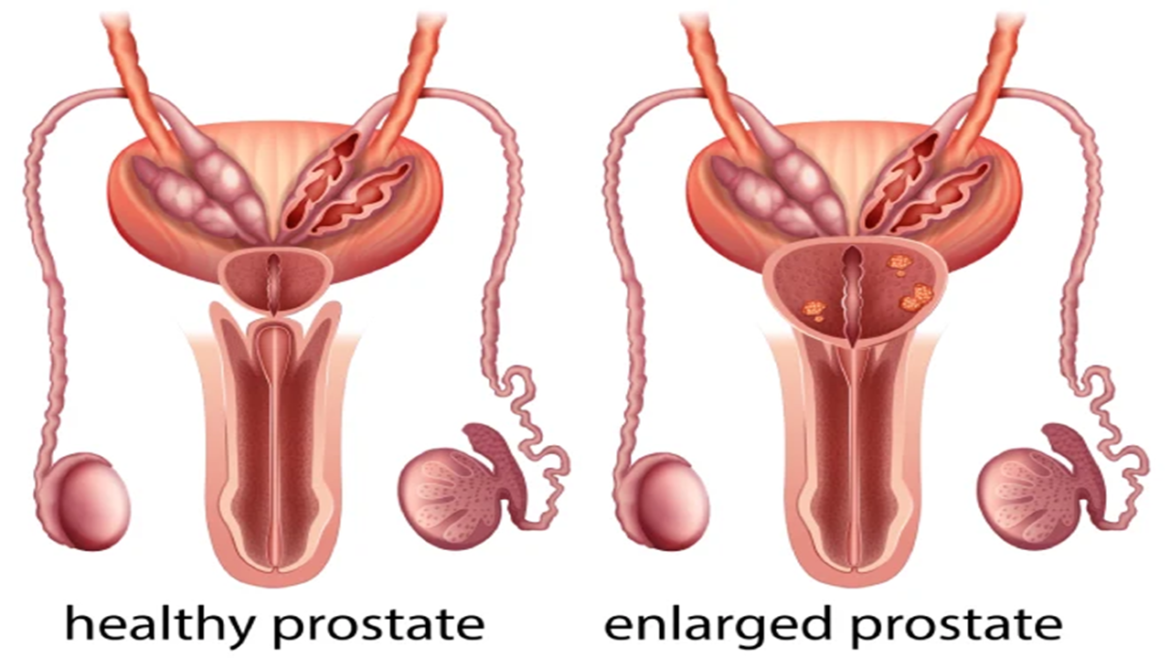
Prostate problems, such as benign prostatic hyperplasia (BPH) and prostate cancer, are widespread conditions that affect a significant number of men worldwide. The percentage of men with BPH and prostate cancer varies depending on age. In general, the risk of both conditions increases with age:
- BPH: The risk of BPH increases significantly after age 50. By age 60, about 50% of men have BPH. By age 80, the prevalence of BPH rises to 80%.
- Prostate cancer: The risk of prostate cancer increases after age 50. By age 65, about 1 in 12 men will be diagnosed with prostate cancer. By age 75, the risk rises to about 1 in 7 men.
- Coexistence of BPH and prostate cancer: BPH and prostate cancer can coexist in the same man. In fact, about 20% of men with prostate cancer also have BPH.
The risk of developing these conditions increases with age. In this article, we will explore the significant advancements in technology that have revolutionized the diagnosis and treatment of prostate problems.
Improved Imaging and Diagnostic Tools
Improved imaging and diagnostic tools have revolutionized the diagnosis and management of prostate problems. These advancements have greatly enhanced the accuracy of detection, localization, and characterization of prostate abnormalities. These advancements have greatly enhanced the accuracy of detection, localization, and characterization of prostate abnormalities. Here are some notable improvements:
- Multiparametric Magnetic Resonance Imaging (mpMRI): mpMRI combines various imaging sequences, including anatomical, functional, and diffusion-weighted imaging, to provide detailed information about the prostate and any suspicious areas. It enables radiologists to detect and characterize tumors within the prostate gland more accurately.
- MRI-Ultrasound Fusion Biopsy: This technique combines the real-time imaging capabilities of ultrasound with the detailed anatomical information from mpMRI. By overlaying the MRI images onto the ultrasound images, urologists can accurately target suspicious areas within the prostate during a biopsy. MRI-ultrasound fusion biopsy improves the accuracy of prostate cancer detection and helps guide treatment decisions.
- Contrast-Enhanced Ultrasound (CEUS): CEUS is a technique that involves injecting a contrast agent into the bloodstream and using ultrasound to visualize the blood flow within the prostate. It helps differentiate between benign and malignant tissues and can aid in the characterization of suspicious areas.
- Prostate-Specific Membrane Antigen (PSMA) PET/CT Imaging: PSMA is a protein highly expressed on the surface of prostate cancer cells. PET/CT imaging using PSMA-targeted radiotracers allows for highly sensitive and specific detection of prostate cancer lesions, including small or metastatic lesions that may be missed by other imaging methods. PSMA PET/CT imaging plays a crucial role in staging, restaging, and detecting recurrent prostate cancer.
- Liquid Biopsy: Liquid biopsy involves analyzing blood or urine samples for specific biomarkers associated with prostate cancer. It provides a non-invasive alternative to traditional tissue biopsies and can offer real-time information about tumor progression, treatment response, and the emergence of treatment-resistant mutations. Liquid biopsies hold promise for monitoring disease status, guiding treatment decisions, and detecting minimal residual disease or recurrence.
These improved imaging and diagnostic tools have significantly enhanced the ability to detect, stage, and monitor prostate problems. They enable more precise and personalized treatment planning, leading to improved patient outcomes, reduced unnecessary procedures, and enhanced overall management of prostate conditions. It’s important to consult with healthcare professionals experienced in utilizing these advanced techniques to ensure the most appropriate diagnostic approach for each individual case.
Minimally Invasive Surgical Techniques
Technological advancements have led to less invasive surgical procedures for prostate problems, resulting in reduced patient discomfort, hospital stays, and recovery time. Techniques such as Urolift, aqua blasting, and eco laser have gained popularity due to their excellent results with minimal side effects. These technologies offer improved outcomes, including reduced blood loss, shorter hospital stays, and faster recovery for patients undergoing prostatectomy.
- UroLift: UroLift is a minimally invasive procedure used to treat benign prostatic hyperplasia (BPH). It involves the placement of small implants in the prostatic urethra to lift and hold the enlarged prostate lobes, thereby opening the urethra and relieving urinary symptoms. UroLift is typically performed as an outpatient procedure and offers the advantage of preserving sexual function and ejaculatory function compared to traditional surgical methods.
- Aquablation: Aquablation is a newer minimally invasive technique for the treatment of BPH. It utilizes a robotic system that combines real-time ultrasound imaging with a high-velocity waterjet to precisely remove excess prostate tissue. This technique allows for targeted and controlled removal of prostate tissue while preserving the surrounding structures. Aquablation offers a balance between efficacy and safety in BPH treatment, with potential benefits in terms of symptom relief and preservation of sexual function.
- Laser Techniques: Laser-based procedures have gained popularity in the treatment of prostate problems. Two common laser techniques used are:
- GreenLight Laser Therapy (PVP): GreenLight Laser Therapy involves the use of a laser to vaporize or remove excess prostate tissue that causes urinary obstruction in BPH. The laser emits high-energy green light that is absorbed by the prostate tissue, leading to its vaporization. This procedure provides effective symptom relief with minimal bleeding and a shorter recovery time compared to traditional surgery.
- Holmium Laser Enucleation of the Prostate (HoLEP): HoLEP is a laser-based technique used for the treatment of both BPH and prostate cancer. It involves the removal of the inner part of the prostate gland using a holmium laser. HoLEP allows for precise removal of prostate tissue while minimizing the risk of complications. It has demonstrated excellent long-term outcomes and is particularly suitable for patients with larger prostate glands.
Focused Ultrasound Therapy
Focused Ultrasound Therapy, specifically High-Intensity Focused Ultrasound (HIFU), is a non-invasive treatment for localized prostate cancer. It uses precisely focused ultrasound waves to heat and destroy cancerous tissue within the prostate. The procedure involves planning based on imaging, targeting the tumor with focused ultrasound waves, and monitoring in real-time. During the HIFU procedure, the patient lies on a table, usually under anesthesia or sedation. The ultrasound transducer, which emits the focused ultrasound waves, is positioned near the patient’s perineum (the area between the scrotum and anus). The focused ultrasound waves are precisely aimed at the cancerous areas identified on the pre-procedure imaging. The waves pass harmlessly through the surrounding tissues until they converge at the focal point within the prostate, where they generate heat. The high-intensity ultrasound energy raises the temperature in the targeted region, causing thermal ablation. The intense heat destroys the cancer cells, leading to their death.
The benefits of focused ultrasound therapy include being non-invasive, precise targeting, preservation of function, and being an outpatient procedure. However, eligibility and suitability should be determined by a healthcare professional based on the individual’s condition.
Advancements in Radiation Therapy
Advancements in radiation therapy have significantly improved the effectiveness and precision of treatment for prostate cancer. These advancements include techniques such as Intensity-Modulated Radiation Therapy (IMRT), Image-Guided Radiation Therapy (IGRT), Stereotactic Body Radiation Therapy (SBRT), and Proton Therapy.
- Intensity-Modulated Radiation Therapy (IMRT): IMRT delivers radiation beams with varying intensities, allowing for precise targeting of the tumor while minimizing radiation exposure to surrounding healthy tissues. This technique uses computer-controlled linear accelerators to shape the radiation beams and deliver them from multiple angles. IMRT enables a high dose of radiation to be delivered to the tumor while sparing nearby organs, reducing side effects.
- Image-Guided Radiation Therapy (IGRT): IGRT involves the use of real-time imaging techniques, such as X-rays or CT scans, to precisely locate and track the tumor before and during treatment. This technology helps compensate for organ motion and ensures accurate targeting. By adapting the radiation delivery based on the tumor’s position at the time of treatment, IGRT enhances the precision and effectiveness of radiation therapy.
- Stereotactic Body Radiation Therapy (SBRT): SBRT delivers highly precise and potent radiation doses to the tumor in a limited number of treatment sessions. This technique uses advanced imaging and computerized planning to deliver high doses of radiation with extreme accuracy. SBRT is typically completed in a few sessions, offering convenience and reducing the overall treatment duration.
- Proton Therapy: Proton therapy is a form of external beam radiation therapy that uses protons instead of X-rays to target and treat prostate tumors. Protons have unique physical properties that allow for precise targeting and depositing the majority of their energy at the tumor site, reducing radiation exposure to healthy tissues surrounding the prostate. Proton therapy may be particularly beneficial for patients with localized prostate cancer, as it can potentially reduce long-term side effects.
Advancements in radiation therapy have resulted in improved tumor control rates and reduced side effects. These techniques offer more accurate dose delivery, better sparing of healthy tissues, and increased treatment precision. As a result, patients may experience fewer complications, improved quality of life, and enhanced cancer control outcomes.
Emerging Technologies
In addition to the aforementioned advancements, emerging technologies continue to shape the landscape of prostate problem treatments.
- Smart patches hold great promise in the field of wearable electronics for healthcare, enabling personalized and proactive management of prostate problems. Smart patches, developed by research groups such as the Sheng Xu Research Group at UC San Diego, utilize flexible and stretchable electronics to continuously collect data and provide real-time feedback to healthcare providers, enabling personalized and proactive management of prostate problems.
- Artificial Intelligence (AI) and machine learning algorithms are being developed to improve diagnostic accuracy, risk stratification, and treatment planning for prostate problems.
- Liquid biopsy offers a non-invasive alternative to traditional tissue biopsies and provides real-time information about tumor progression and treatment response. Liquid biopsy can provide a more comprehensive picture of the disease, allowing for personalized treatment decisions.
- Immunotherapy and targeted therapies are two distinct but interconnected approaches to cancer treatment that have revolutionized the field of oncology. While they have different mechanisms of action, both aim to specifically target cancer cells while minimizing damage to healthy tissues. Thus far, they have shown promising results in the treatment of advanced or metastatic prostate cancer.
In conclusion, technological advancements have significantly improved the diagnosis and treatment of prostate problems. These innovations, ranging from improved imaging and diagnostic tools to minimally invasive surgical techniques, focused ultrasound therapy, and advancements in radiation therapy, have enhanced patient outcomes and quality of life. As emerging technologies continue to evolve, there is great potential for further advancements in the field, offering new possibilities for personalized and effective prostate problem management.
References:
- Mottet, N., et al. (2021). EAU Guidelines: Prostate Cancer. European Association of Urology. Retrieved from https://uroweb.org/guideline/prostate-cancer/
- Cornford, P., et al. (2021). EAU Guidelines: Non-neurogenic Male LUTS. European Association of Urology. Retrieved from https://uroweb.org/guideline/non-neurogenic-male-luts/
- Zaorsky, N. G., et al. (2020). Proton therapy use in the treatment of prostate cancer in the United States: Patterns of care and comparative effectiveness. International Journal of Radiation Oncology, Biology, Physics, 107(1), 146-157.
- Rosenkrantz, A. B., et al. (2018). Prostate magnetic resonance imaging and magnetic resonance imaging targeted biopsy in patients with a prior negative biopsy: a consensus statement by AUA and SAR. Journal of Urology, 199(2), 749-758.
- Rowe, S. P., et al. (2018). PSMA-based [(18)F]DCFPyL PET/CT is superior to conventional imaging for lesion detection in patients with metastatic prostate cancer. Molecular Imaging and Biology, 20(6), 1021-1024.
- Wyatt, A. W., et al. (2017). Liquid biopsies for monitoring metastatic prostate cancer. Nature Reviews Clinical Oncology, 14(2), 109-127.
- Ahmed, H. U., et al. (2017). Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. The Lancet, 389(10071), 815-822.
- Woo, H. H., et al. (2016). Focused ultrasound as a non-invasive procedure for cancer therapy. Medical Journal of Australia, 205(10), 473-477.
- Siddiqui, M. M., et al. (2015). Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA, 313(4), 390-397.
- Roehrborn, C. G., et al. (2013). Efficacy and safety of a new minimally invasive treatment for symptomatic benign prostatic hyperplasia: Aquablation of the prostate. BJU International, 111(7), 1131-1137.
Disclaimer: “This blog post was researched and written with the assistance of artificial intelligence tools.”